With an incidence rate of approximately 1.9%, Achilles tendon injuries, consisting of ruptures and tendinopathies, do not occur particularly frequently amongst footballers. But this is an important topic because of the long period of recovery associated with this type of injury. It transpires that Achilles tendon injuries are one of the top 4 injuries requiring the longest recovery time in football. Only an anterior cruciate ligament rupture, cartilage problems and tibia/fibula fractures have a longer average injury recovery time. Achilles tendon injuries may not be common, but they do have a huge impact on the player and the team. Sufficient knowledge about the diagnosis, treatment and recovery is therefore important.
Achilles tendinopathies
An Achilles tendinopathy is hallmarked by localised load-dependent pain around the Achilles tendon. There are two types: the mid-portion Achilles tendinopathy and insertion Achilles tendinopathy (see Figure 1). The exact location of the symptoms determines the type of tendinopathy. The new guideline ‘Achilles tendinopathy’ recommends the following criteria when making a diagnosis:
Mid-portion Achilles tendinopathy
Make the diagnosis of mid-portion Achilles tendinopathy based on the presence of all of the findings listed below:
● Symptoms localised to 2 to 7 cm proximal to the Achilles tendon insertion.
● Painful Achilles tendon mid-portion in relation to sport/non-sport loads.
● Local inflammation of the mid-portion Achilles tendon (this can be absent if symptoms have been present for only a short period of time).
● Pain on local palpation of the mid-portion Achilles tendon.
Insertion Achilles tendinopathy
Make the diagnosis insertion Achilles tendinopathy based on the presence of all of the findings listed below:
● Symptoms localised in the Achilles tendon insertion region (first 2 cm form the insertion of the Achilles tendon).
● Painful Achilles tendon insertion in relation to sport/non-sport loads.
● Local inflammation of the Achilles tendon insertion (this can be absent if symptoms have been present for only a short period of time).
● Pain on local palpation of the Achilles tendon insertion.

Insertion Achilles tendinopathy – Mid-portion Achilles tendinopathy
Figure 1. Subclassification Achilles tendinopathy. Taken from: Guideline Achilles Tendinopathy presentation
Past experience shows that many disorders were mistakenly diagnosed as Achilles tendon injuries. Figure 2 shows possible alternative differential diagnoses. The number of differential diagnoses in a relatively small area demonstrates the complexity of the correct diagnosis. However, this diagnosis is essential, as it directs the focus of the treatment plan.
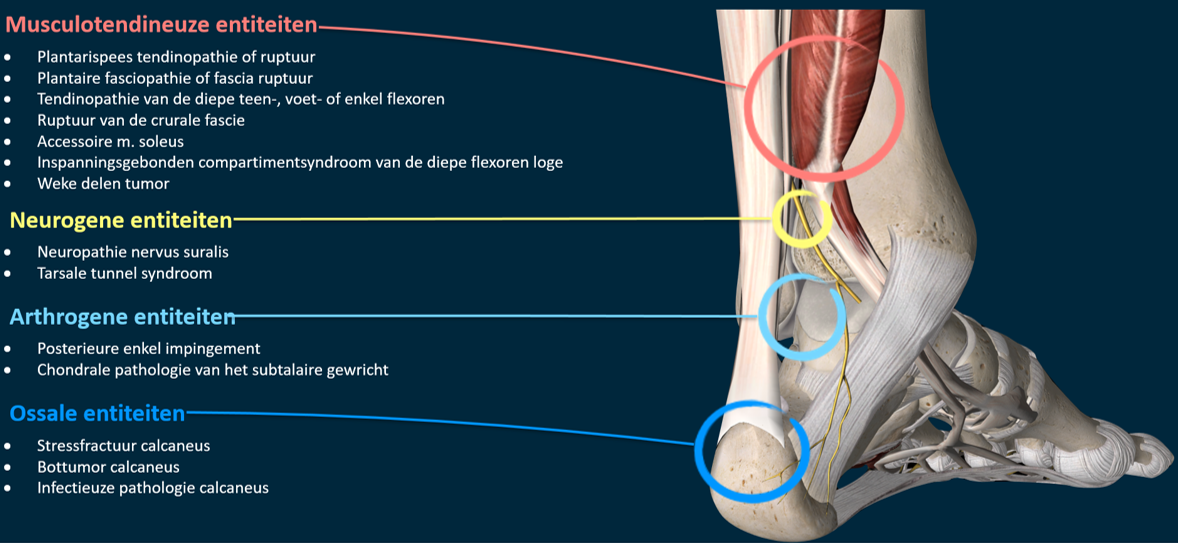
Musculotendinous entities
• Plantar tendinopathy or rupture
• Plantar fasciopathy or fascia rupture
• Tendinopathy of the deep toe, foot or ankle flexors
• Rupture of the crural fascia
• Accessory soleus muscle
• Exercise-induced compartment syndrome of the deep flexor compartment
• Soft tissues tumour
Neurogenic entities
• Sural nerve neuropathy
• Tarsal tunnel syndrome
Arthrogenic entities
• Posterior ankle impingement
• Chondral pathology of the subtalar joint
Ossal entities
• Calcaneal stress fracture
• Bone tumour of the calcaneus
• Infectious calcaneal pathology
Figure 2. Differential diagnoses Achilles tendinopathy. Taken from: Guideline Achilles Tendinopathy presentation
What is actually done in practice with Achilles tendinopathy?
Experience has shown that many footballers are hesitant about Achilles tendon symptoms. Possibly because the constraints during the initial phase of the sporting activity are still minor and/or the injury builds up gradually without an acute episode. However, the Achilles Tendinopathy guideline recommends an active approach. This approach is supported by the latest literature. The main rule here is to keep the load and tolerance in balance. This can be done by temporarily ceasing the provoking sport load and possibly replacing this with non-provoking sport load (e.g. cycling/swimming instead of no/less football training). Gradual build-up of the sport load is crucial in this respect. But when are the load and tolerance properly balanced? In general, during and immediately after playing sport, a pain score of 0 to 5 is acceptable (see Figure 3). If this level of pain reduces during the subsequent hours and, also if only slight limitations are present the following morning. The VISA-A questionnaire can also be used to monitor development of the symptoms.
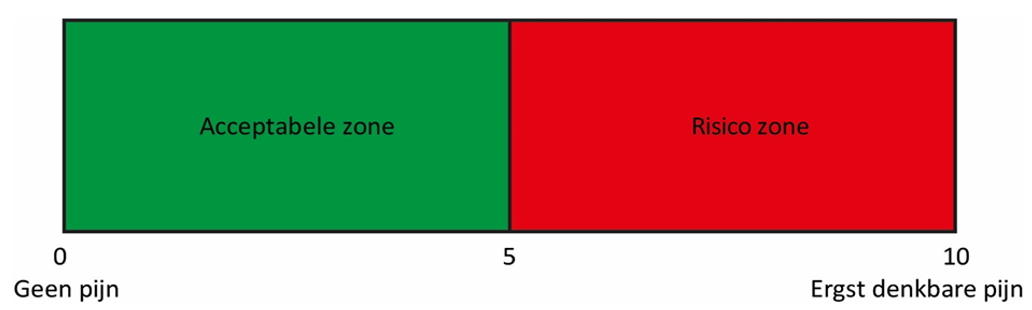
Acceptable zone – Risk zone
No pain – Worst pain imaginable
Figure 3. Pain monitoring. Taken from: Achilles Tendinopathy Guideline
Reduced calf muscle strength is associated with Achilles tendon symptoms. The advice is therefore to offer an eccentric strengthening exercise programme which builds up gradually, lasting at least 12 weeks, in addition to the modifications in load/tolerance. As yet, there is no conclusive evidence about the best exercises, but you will find a basic exercise schedule here. Adhering to the exercises consistently and finding the right load/tolerance balance are therefore essential for the treatment of Achilles tendinopathies.
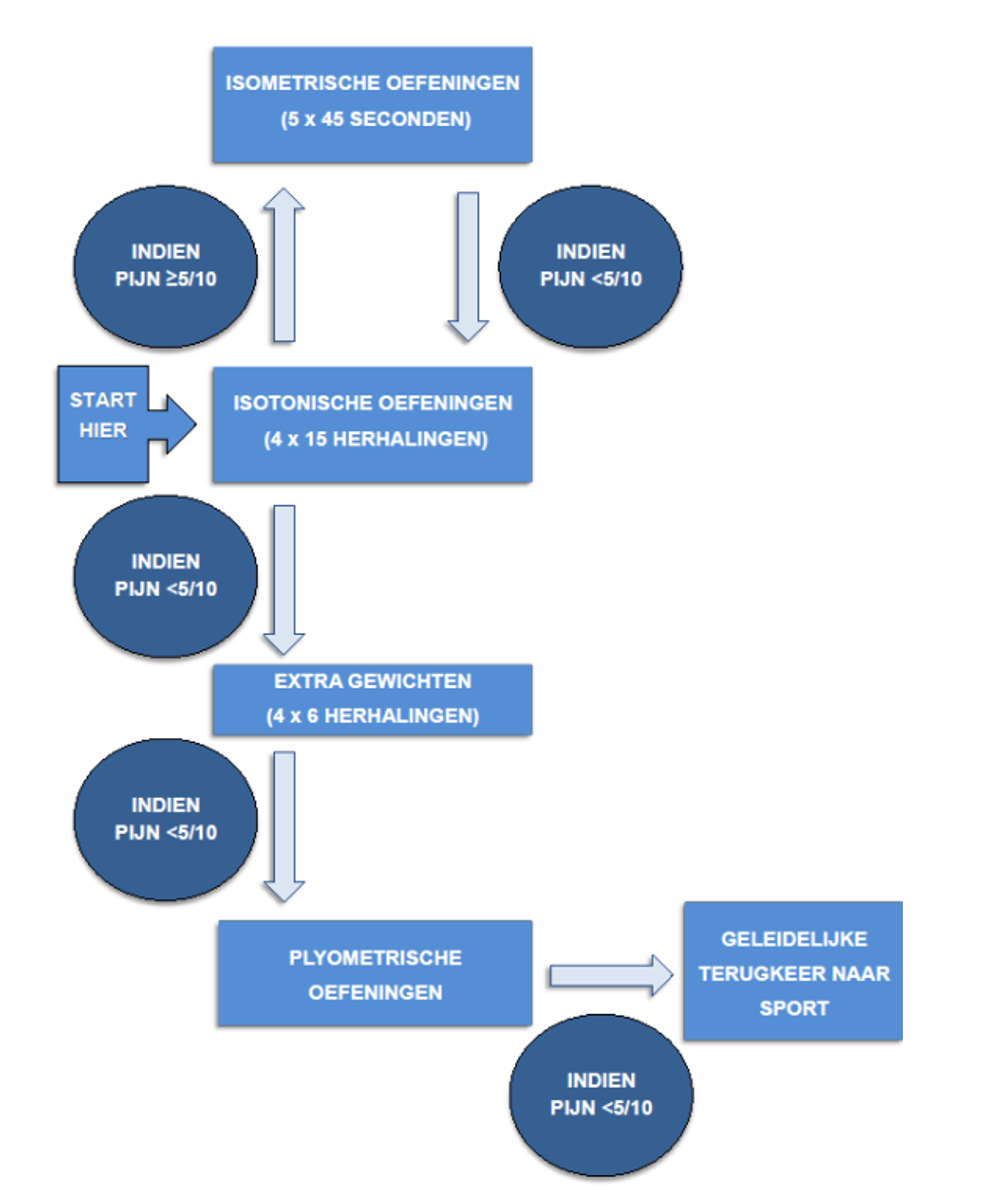
Isometric exercises (5 x 45 seconds)
If pain ≥ 5/10 If pain < 5/10
Start here Isotonic exercises (4 x 15 repeats)
If pain ≥ 5/10
Additional weights (4 x 6 repeats)
If pain < 5/10
Plyometric exercises
Gradual return to sport
If pain < 5/10
Figure 4. Advice is to build up exercise therapy. Taken from: Achilles Tendinopathy Guideline
If there is an insertion Achilles tendinopathy, significant dorsiflexion angles of the ankle can lead to increased pain as a result of additional compression on the calcaneus and retrocalcaneal bursitis. Shoes can also cause additional pressure. In this case, consider training on a flat surface with and without shoes during the initial stage.
Get started!
Take an active approach with footballers with Achilles tendon symptoms. Do not simply ‘wait and see’. Provide advice based on the load and tolerance and teach the footballer how he/she can monitor this himself/herself. In the event of Achilles tendinopathy, complete rest is often not the right solution. Practise daily living activities and play sport within the acceptable pain scores and start with a strength programme which builds up gradually for the calf muscles, such as the Alfredson protocol.
1 Ekstrand J, Krutsch W, Spreco A, et al Time before return to play for the most common injuries in professional football: a 16-year follow-up of the UEFA Elite Club Injury Study British Journal of Sports Medicine 2020;54:421-426.
2 Bahr R, Clarsen B, Ekstrand J Why we should focus on the burden of injuries and illnesses, not just their incidence British Journal of Sports Medicine 2018;52:1018-1021.
3 Vereniging voor Sportgeneeskunde. (2020, 15 oktober). Diagnose van achilles tendinopathie - Richtlijn - Richtlijnendatabase. Richtlijnendatabase. https://richtlijnendatabase.nl/richtlijn/achilles_tendinopathie/startpagina_-_achilles_tendinopathie.html
4 van der Vlist, A. C., Winters, M., Weir, A., Ardern, C. L., Welton, N. J., Caldwell, D. M., Verhaar, J., & de Vos, R. J. (2021). Which treatment is most effective for patients with Achilles tendinopathy? A living systematic review with network meta-analysis of 29 randomised controlled trials. British journal of sports medicine, 55(5), 249–256. https://doi.org/10.1136/bjsports-2019-101872